Australia: The Care Together Program
CICOPA interview with Melina Morrison, CEO BCCM, and Gillian McFee, Care Together Program Manager.
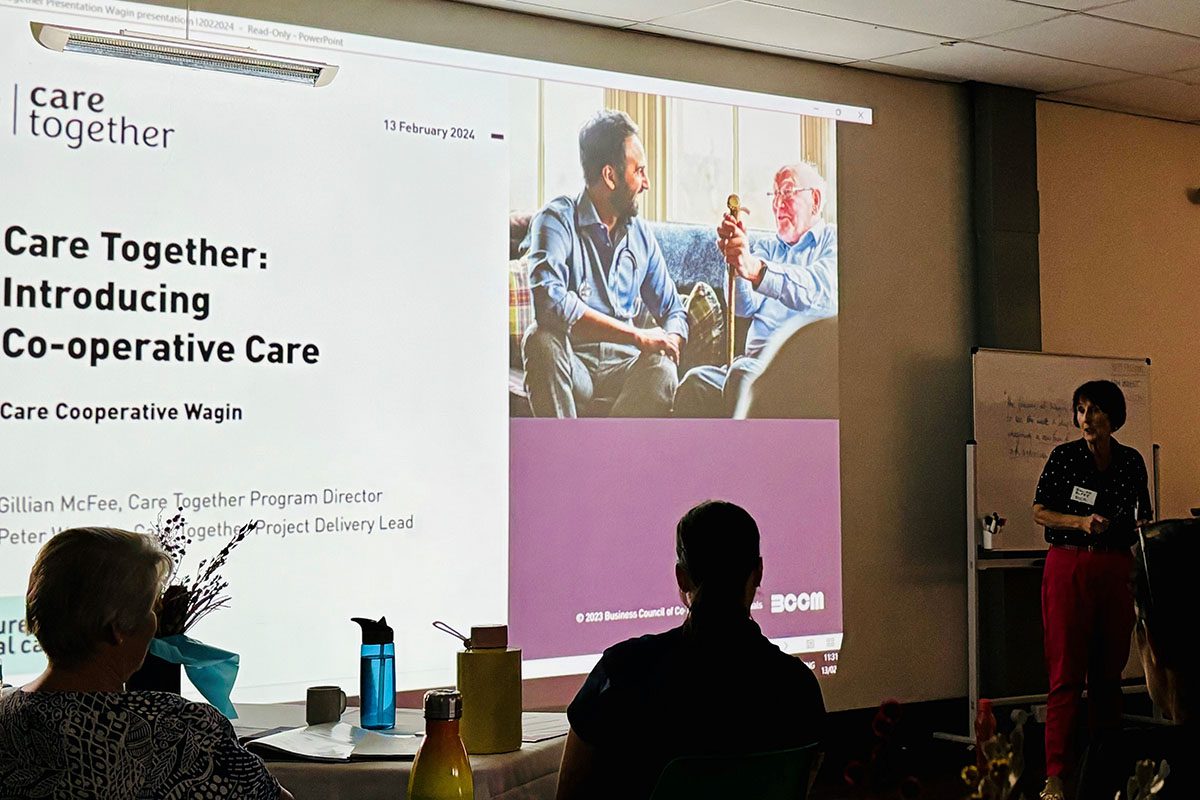
CICOPA had the chance to sit down with Melina Morrison, CEO, and Gillian McFee, Care Together Program Manager from the Business Council of Cooperatives and Mutuals (BCCM), CICOPA’s Australian member.
This article was republished with permission from CICOPA and was originally published in the August 2023 edition of CICOPA’s Work Together newsletter.
BCCM has recently received an A$7 million grant from the Australian Government Department of Health and Aged Care to implement the Care¹ Together Program in order to create and strengthen care cooperatives as a solution to the challenges in Australia’s care sector especially in markets where service delivery is failing including regional, remote and rural communities. The program will run from January 1, 2023, until June 30, 2025.
CICOPA: What is the care landscape at the moment in Australia?
BCCM: The Australian care landscape is one of increasing demand. The aging demographic profile of Australia is contributing to a looming crisis in workforce shortages. The care sector is the largest and fastest-growing part of our economy; in the Australian federal budget, we are looking at expenses exceeding A$200 billion in the care sector.
The sector is facing worker shortages, for two main reasons. Firstly, carers in Australia are mainly middle and older-aged women, which will lead to worker shortages as they retire in the coming years.
Secondly, due to COVID-19 there has been a sharp drop in the arrival of migrant workers, who are another major demographic worker group in the care sector.
In recent years, a number of inquiries and Royal Commissions have uncovered systemic problems in the quality of services and employment in the care sector. The most significant inquiry was the Royal Commission into Aged Care Quality and Safety. The report was damning, calling the situation a “shocking tale of neglect”. In particular, it noted the lack of choice in services – for example, although most older Australians prefer to receive care at home, care services are instead focused on residential care models. The report also highlighted the increased privatization within the sector, which leads to large profit-lead enterprises in the system for financial benefit. Consequently, the value generated does not remain in the sector and is not reinvested to improve care for consumers and working conditions for care employees. Another critical issue is that carers’ wages are insufficient to support a reasonable standard of living.
Finally, the report also raised questions about the lack of innovation, in terms of both service provision and ownership structures of care enterprises. These problems have a heightened impact in rural, regional, and remote Australia, since care services there are already inadequate in many locations.
CICOPA: What is the current state of development of care cooperatives in Australia?
BCCM: We can give two readings of the situation. On one side, we are beginning to develop care cooperatives in Australia. The discussion has only recently started, and there is no specific sector of care cooperatives in Australia. On the other side, some successful care cooperatives already exist that organically emerged in response to the needs of workers in the sector. For example, there are around 30 Aboriginal community-controlled services within the Indigenous cooperative movement.
The worker cooperative model is not common in Australia. Historically, this model was hindered by a lack of an enabling legislative environment, a poor understanding of the cooperative model in policy and business circles, a lack of a national peak body for the sector, and the dominance of trade unions as the preferred method of worker organisation. However, in recent years we have started to see change.
Industrial relations are starting to change due to the casualization of labour (e.g. the rise of platform work), which means trade unions need capacity to organise and protect freelance workers. Moreover, we have a care sector that is in urgent need of a major overhaul especially to attract and retain workers in high quality and dignified care jobs. These factors mean that current conditions are favourable for more care cooperatives to form in Australia.
CICOPA: How did the Care Together Program come to be?
BCCM: It has taken a decade of advocacy, really. We had to start by building a story about the purpose of cooperatives in the Australian context and raising awareness about cooperatives as an alternative, people-centred business model and their potential to provide services in the care sector.
Our strategy was to go in and ask: “What is the problem you are trying to address?”, and “Have you thought of cooperative and mutual solutions?” With few domestic examples, we really depended on the experiences from the international cooperative community. Our context of rising demand and increasing privatization opened an opportunity for cooperatives to take shape. In particular, cooperatives can partner with governments to deliver care, while keeping value and reinvestment in the health and care sector.
When the Royal Commission into Aged Care clearly stated that the care system was broken, we saw this as an opportunity to show that cooperatives could help. We proposed that the Government invest in education and information about cooperative and mutual enterprise models to help address the recommendations of the Royal Commission.
CICOPA: What is the goal of the Care Together Program?
BCCM: Our goal is “dignified, safe and quality social care for vulnerable people in all settings, including regional, rural and remote communities delivered by empowered and well-trained workers in decent jobs”. Care Together is an education, advisory and support program that will assist successful projects to develop sustainable service delivery in areas where current approaches are failing, including a focus on regional, rural and remote parts of Australia. Cross-sector, multi-disciplinary models will be an important focus of the Care Together Program and aligned to these high-level program outcomes:
Supporting the establishment of innovative models of social care delivery (including aged care, disability care, veterans’ care, Indigenous services, allied health and primary care) in areas where current approaches are not working.
Increasing opportunities for providers of social care to transition to co-operative and mutual models to address workforce challenges and improve service delivery.
In terms of projects, Care Together will support the development of new cooperatives or mutuals to deliver care, support growth and scaling projects working with existing cooperatives and mutuals, and facilitate the co-design and development of a user-tested prototype to establish a digitally enabled member-owned cooperative to support service delivery in areas of unmet need by providing back-office functions and other collaborative solutions for smaller providers.
Around all of this, we will be engaging in research – we want to ensure we obtain high- quality data about the successes and challenges of the program. Furthermore, we want to build case studies from each project to better understand how to make social care cooperatives successful.
We are using the Mutual Value Measurement Framework© to measure the total value creation of the new and growing cooperatives we are assisting. This ensures that the framework for measuring the success of the projects is informed by the unique characteristics of cooperatives themselves.
CICOPA: Based on the challenges for care workers and beneficiaries, that you identified above, how is the program addressing them?
BCCM: The program focuses on empowering those providing the care, and those receiving it, because they are the most important yet the least empowered people under the current system. On the worker side, for example, we have a project for a primary health network in regional, rural, and remote Australia. It is a multidisciplinary health and care team delivering services to a small town of 30,000 people, with several outlying smaller communities. They approached us to learn how their organisation might look as a cooperative. This plan is likely moving forward, and other primary health networks are showing interest in the cooperative model as a result.
On the other hand, we have a project for people with high support needs due to disability. The goal of the program is to facilitate a better living situation for young people who have been inappropriately placed in aged care homes because of these support needs. The project is a cooperative that aims to return choice to the people who are the beneficiaries of care – the cooperative model allows them to pool their disability funding resources and achieve a greater degree of autonomy.
CICOPA: How will BCCM and the program ensure the sustainability of the established new cooperatives?
BCCM: Many small cooperatives in their infancy need cooperative development and business advice to enable them to scale up and operate sustainably. In a period of two years, we’ll only be able to get them going. In order to survive, they’ll need support from the cooperative movement, so we facilitate them becoming BCCM members. The measurement system we have designed, Mutual Value Measurement, allows them to show how their purpose is driven by their business performance. We want to make sure that they demonstrate how they are delivering value and thus helping the community. We also want to make sure that cooperatives are sustainable, so access to capital is very important. In Australia, we have worked very hard to develop innovative ways for raising capital. As a result, cooperatives can use specially designed capital instruments to raise vital equity capital without sacrificing their cooperative ethos.
Our program is open to anyone from around the world to follow online. Visit caretogether.coop to find more about our Social Care Community of Practice.
CICOPA: Thank you for your time!
Related case studies
Discover how co-ops and mutuals are making a big impact in Australia’s health, community and social services sector, successfully delivering high-quality services and support to those who need it most.Find a care co-op or mutual near you
Use our new interactive map to find care co-ops and mutuals across Australia.